A home-based exercise programme for people with peripheral arterial disease - COVID-19 special edition:
What is the aim of this document and who is it for?
The aim of this document is to provide detailed exercise guidance for people with intermittent claudication during the COVID-19 outbreak; a cramping/pain/ache that comes on in the calves, thighs and/or buttocks when walking that is caused by peripheral arterial disease (PAD). Due to the current outbreak of Covid-19, opportunities for exercise are limited, especially in a formal setting. These exercises may be done at home or in the local community, paying close attention to the Government’s COVID-19 social distancing measures. Regular supervised exercise is a recommended treatment for people with intermittent claudication, but the social distancing measures may stop you from attending an exercise class. This may leave you wondering what you can do in your own time to help your legs. This guide will help you to find alternative ways to stay active and reduce the pain you get in your legs without the need for specialised equipment or facilities.
Have patients been involved in designing this document?
Yes. This document was designed following discussions with our patient and public involvement group, which includes several patients with intermittent claudication who have participated in a supervised exercise programme. One member of this group also provided specific feedback on this document.
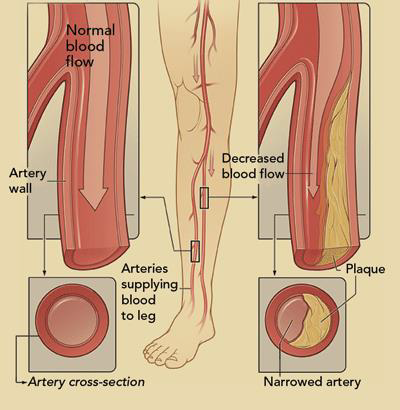
What is peripheral arterial disease?
Peripheral arterial disease is a form of cardiovascular disease caused by a build-up of fatty plaques in the blood vessels that supply the legs. The accumulation of these deposits happens over a long period of time and may cause no issues and go unnoticed until the arteries become so narrow that blood flow to the muscles becomes limited.
PAD is one of the most common forms of vascular disease. Roughly 1 in 10 people have PAD, which can sometimes cause painful legs when walking, but can progress to cause painful legs when resting, skin ulcers and gangrene.
What is intermittent claudication?
Intermittent claudication is a symptom of PAD, where a lack of blood flow to the legs during walking can cause discomfort/pain in the calves and other parts of the leg. People experience this “pain” differently; they also describe it as an ache, cramping sensation, numbness or heaviness. For simplicity we will refer to it as a pain in this document. The pain builds during walking to the point where you need to stop and rest. The pain typically disappears within 1-5 minutes of resting. If you walk faster, uphill or on uneven surfaces the pain will come on more quickly. If you walk more slowly, the pain will come on slower, but this pace might be frustratingly slow. Intermittent claudication is the name given to this type of pain. Intermittent claudication can be disabling and stop people from doing everyday tasks like shopping, gardening or participating in social activities.
What is going to happen to my legs?
In the vast majority of cases PAD remains clinically stable for years without treatment though the claudication pain people experience can vary over time. A small proportion of people get progressively worse, which can mean more frequent or severe pain and worsening walking ability.
What can I do about it?
There are two main recommendations for managing this condition. Sticking to these can help improve your walking ability and prevent your legs from getting worse:
1. Preventing cardiovascular disease from progressing
This means taking appropriate medications daily (e.g. statins, blood thinners and blood pressure tablets), eating healthily and maintaining a healthy weight. Smoking is particularly harmful to PAD sufferers and must be avoided. These will also reduce your risk of heart attacks or strokes: you are an increased risk of these. Talk to your GP if you need help with these.
2. Exercise
Regular exercise has been shown to improve walking ability and reduce pain in people with PAD by at least as much as a successful operation but without the risks. Some patients get rid of their leg pain through regular exercise alone. However, it is important to appreciate that unlike an operation the effects of exercise are not instantly noticeable. The benefits accumulate slowly, and many people don’t notice that they are improving for around 6 weeks. These benefits are seen in most people, even if they can only walk for 20 metres when they start.
Why exercise helps
Even though you may experience pain in your legs when you push yourself, this is not a sign you should avoid physical activity.
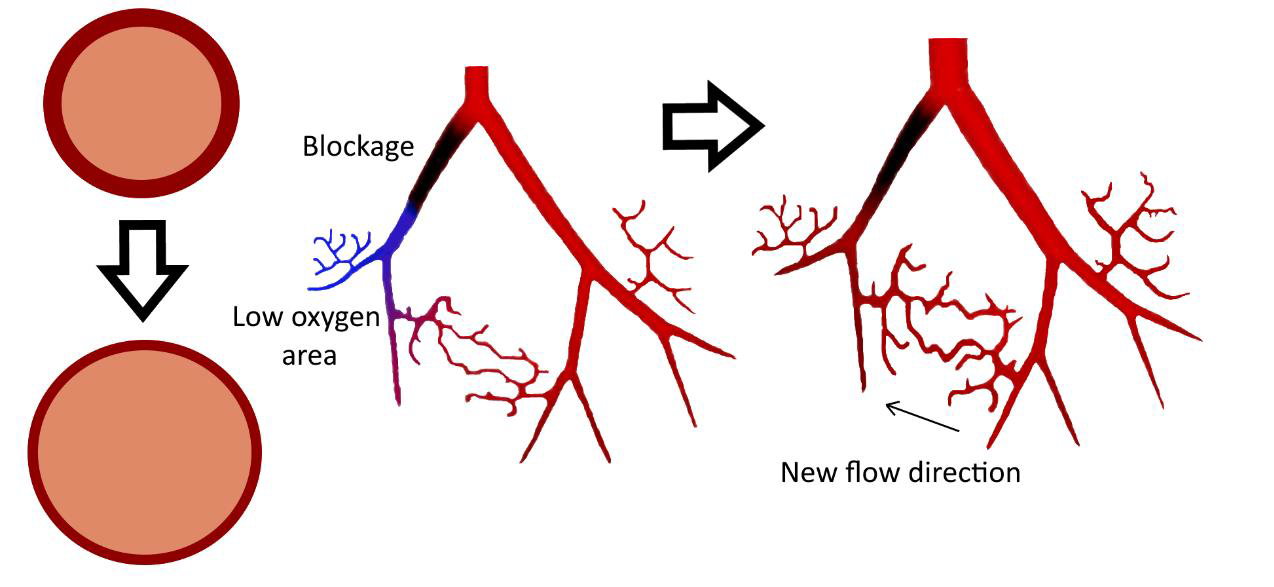
One of the ways to help your blood vessels stay healthy is by repeatedly increasing the blood flow around your body. Exercise does this by increasing your heart rate which causes blood to be pumped around your body faster. Forcing blood around your body sends a signal to your existing blood vessels to open up more and also to grow new blood vessels that can get around areas where blood flow is limited, as shown in the image below. When this happens, more oxygen can get to the muscles in your legs and your leg pain will reduce. This is a slow process that takes place over weeks and months of regular exercise. It can be thought of in the same way that someone may spend several months getting fit to run a marathon. Your body will be adapting to get better at exercising, but the process is so gradual that you won’t typically notice any improvement for 4-6 weeks.
Another way that our bodies change with regular exercise is that we often become fitter. One element of this means that with exercise, the muscles become more efficient and are able to take and use more oxygen from the blood.
What if I don’t think I can do any exercise?
It is very common for people with PAD to have other health issues that may make them feel like exercise is not an option for them. Evidence suggests that the right type of exercise can be helpful for most long-term conditions.
Common conditions that do not prevent engagement in exercise:
- COPD or lung conditions
- Cancer
- Heart conditions (including heart
- Attacks and operations)
- High blood pressure
- Diabetes
- Musculoskeletal conditions
Exercise recommendations
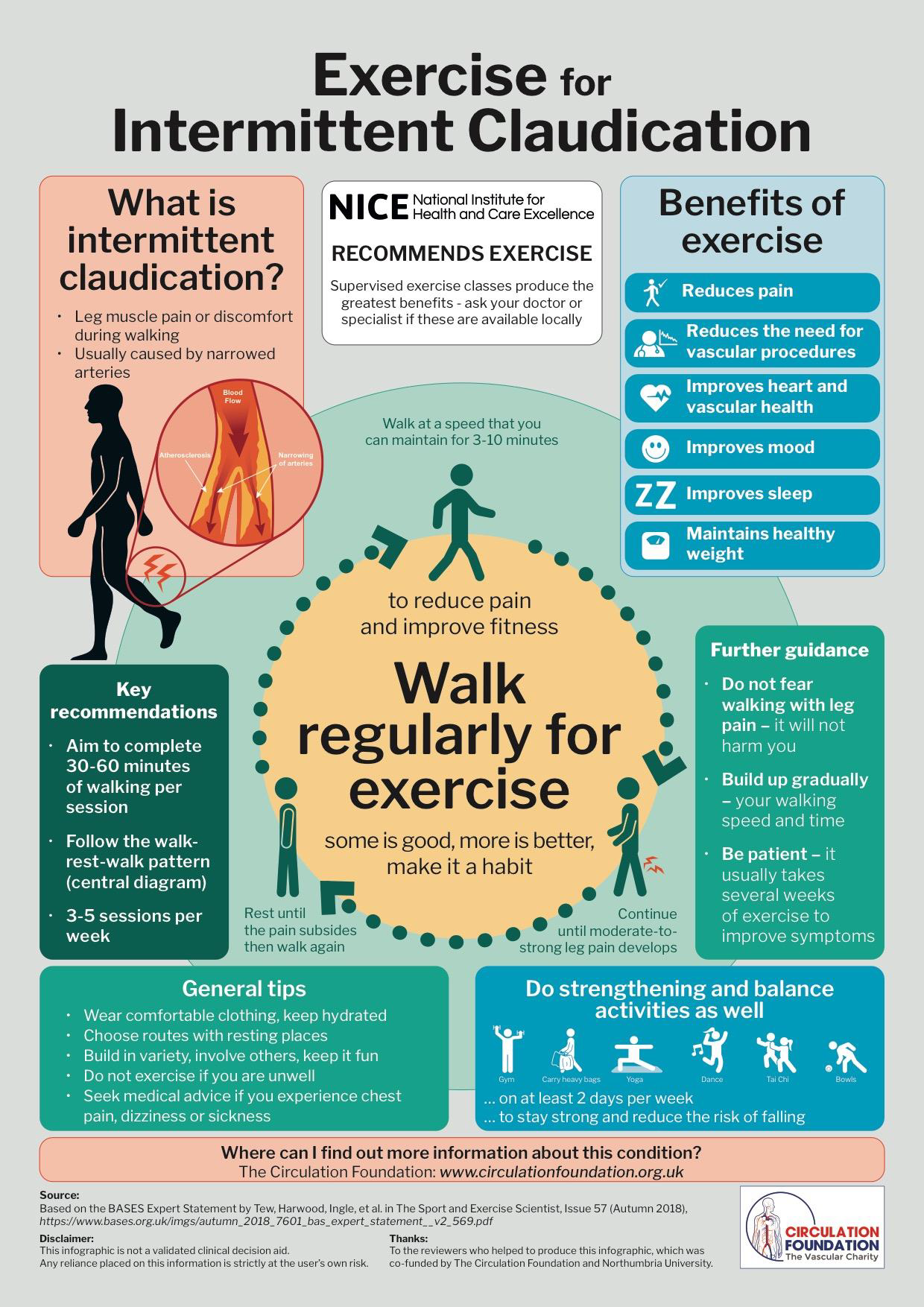
In this section we will describe some of the types of exercise that will benefit you and how you should perform them. A visual summary of the current recommendations can be found on the next page.
Cardiovascular or aerobic exercise, ideally walking, should be performed on most (at least 3-5) days a week, for at least 30, up to 60 minutes per day. Sometimes this may be too much to do in one go and can be broken up into smaller sessions of 10-20 minutes throughout the day.
Resistance or strengthening exercise should also be performed 2 days a week to help with balance and strength. You can use tins of food for weights and perform a number of exercises such as these recommended by Age UK: https://www.ageuk.org.uk/Documents/EN-GB/strength_and_balance_training_PDF.pdf?dtrk=true
It is important to gradually progress how much exercise you do and how hard you do it. This can be as simple as increasing how long you exercise for per day, how many times you exercise in a week or how many times you can perform an exercise without stopping to rest. A good starting point is to try to do 15 minutes of walking at least twice a day and gradually increasing it each week. You should set a goal each week of how long you will try to exercise for and increase it slightly when it has been reached.
Remember, if you are exercising outside, maintain social distancing of at least 2 metres.
See the latest Government guidance here: https://www.gov.uk/government/publications/covid-19-guidance-on-social-distancing-and-for-vulnerable-people
Safety
Before all exercise (either indoor or outdoor), perform a short gradual warm-up to get your body ready for exercise and a gentle cool-down to slow down afterwards. Also, you should wear comfortable but appropriate footwear and clothing and ensure you have adequate space to exercise safely. If you are prescribed an inhaler and/or GTN (angina) spray, keep this with you whilst you exercise.
Outdoor Exercises
Walking
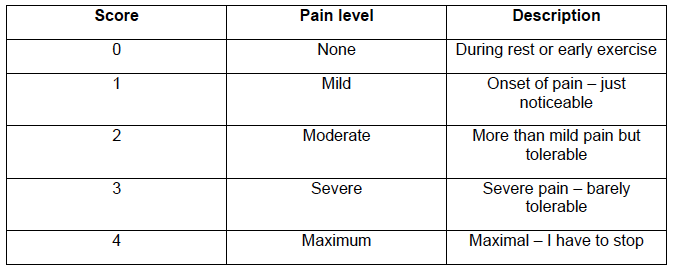
Walking for exercise: it is helpful to routinely try to walk to improve your health as an addition to your normal activities. You should walk at a pace to bring on a moderate to severe level of claudication pain within 3-10 minutes, reaching a score of 2-3 on the scale below, before stopping to rest until it disappears, then walking again. No harm will be caused by continuing to walk with the pain as far as possible. In fact, a moderate amount of pain should be aimed for when walking for exercise. If you can walk for 10 minutes without needing to rest, you should consider walking a little faster, so that you do need to stop within 10 minutes. The duration of your walk should only include time spent walking and not rests, and you should set walking targets to regularly increase how long you walk for. Once you reach 60 minutes per session, you should maintain this and increase it if possible. The infographic on the previous page demonstrates how you should complete your walking exercise.
You don’t always have to walk for exercise. Other exercises such as cycling can also improve your walking, as long as you get your heart pumping faster or get a little breathless for a long enough period of time. Walking is probably best though, and you should try to do this as much as possible.
Cycling
Cycling should also be performed at a moderate pace, enough to make you feel a little breathless and your muscles to ache a little. You can also take breaks when cycling but try to cycle at a speed where you do not need to rest during the session.
Gardening
If you enjoy gardening, you can also make this into exercise by working a little bit faster. You should garden so that you are again a little breathless, but it is easily maintainable. You can take regular breaks here too.
Indoor exercises
A number of exercises can also be completed inside that count towards your daily duration of exercise. The following example circuit of exercises is simple to perform and can be done without any equipment. As always, work at an intensity that makes you a little breathless. You should follow the circuit by performing one aerobic cardiovascular (CV) exercise, followed by an active recovery (AR) exercise, ideally spending 2 minutes on each exercise.
Exercises:
CV 1. Step-up This can be done on any stairs/steps in and around your home. Simply step onto the step with your leading leg, then step up with your back leg so that both feet are on the step, then step off one foot at a time until both feet are on the floor. You may wish to alternate the leading leg. AR 1. Bicep curls Start with your arms by your sides and flex at the elbow bringing your hands up to your shoulders, keeping your upper arms still and your elbows by your sides. You can use tins of food for weight to make this a little more difficult, but nothing too heavy!
CV 2. Marching Walking on the spot at a slightly higher intensity with a set rhythm.
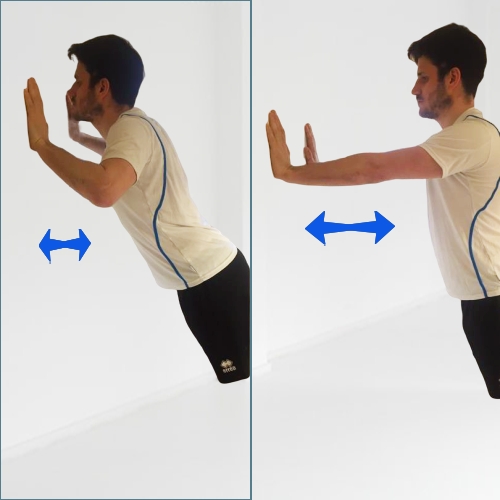
AR 2. Wall press Start in a standing position and place your hands shoulder width apart on a wall at around chest level. You should move your feet back until you are at a slight angle with the wall. Then bend your elbows until your chest is almost at the wall, then straighten your arms again (think press up motion!).
CV 3. Sit-to-stand Start by standing up in front of your chair, with your feet shoulder width apart, and slowly sit down into the chair, maintaining good posture. You should then stand up again, into the same position.
AR 3. Calf raises
Stand with your feet flat on the floor, holding on to something sturdy. Slowly lift your heels off the ground, so you are on your tip-toes and can feel slight tension in the calf then return to standing.
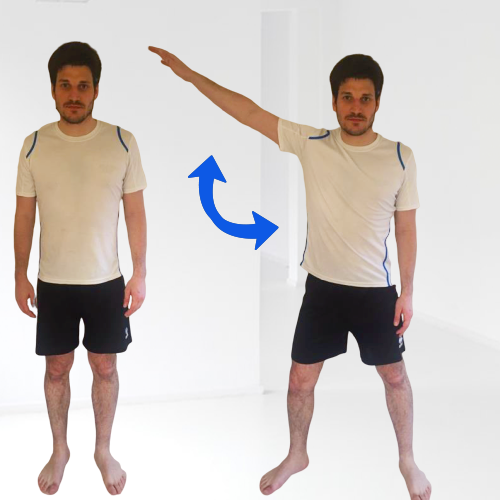
CV 4. Half stars
Stand with your feet shoulder width apart and step one foot out whilst raising your arm to above shoulder height (think half a star jump!), then repeat on the other side.
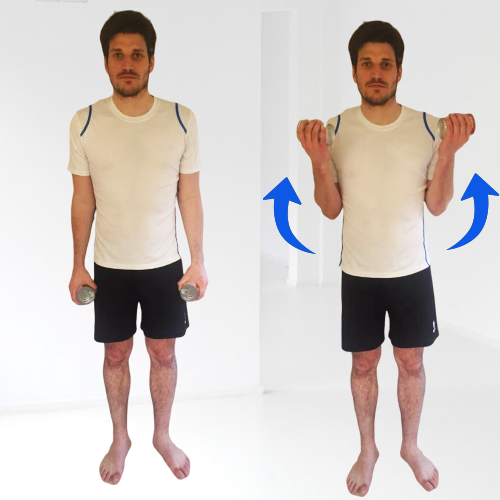
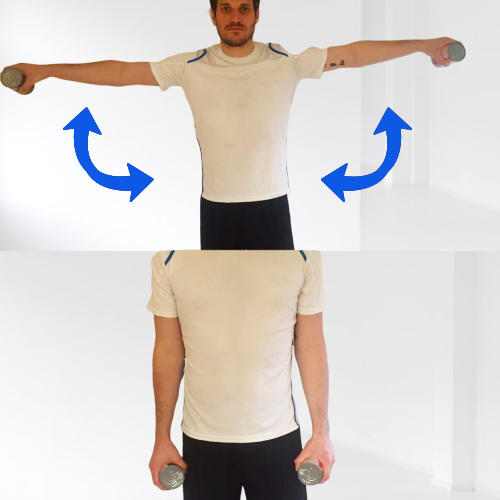
AR 4. Lateral raises
Start with your arms by your sides and raise both arms until they are in line with your shoulders, then lower them down again. You can use tins of food for weight to make this a
little more difficult, but nothing too heavy!
You should repeat the circuit until you have achieved your target time.
CV1. Step Up
CV2. Marching
CV3. Sit-to-stand
CV4. Half Stars
AR 1. Bicep Curls
AR2. Wall Press
AR3. Calf Raises
AR4. Lateral Raises
Setting goals
To help you maintain regular exercise it is helpful to think about what you want to achieve in the long-term. For example, this could be to complete a long countryside walk with a family member. Setting short-term goals can help you achieve this and using the SMART acronym is helpful. SMART means that your goals should be:
- Specific
- Measurable
- Achievable
- Realistic
- Timely
Here are some examples of the types of short-term exercise goals you could set yourself:
- 6000 steps on 5 days of this week and 6500 steps on 5 days next week
- Complete my exercise circuit three times per week for 4 weeks
- Walk for 10 minutes without stopping 3 days this week
- Completing my normal walk in 35 minutes for 3 days this week
- Stop only 3 times on my normal walk for 3 days this week
- Walk all the way to the shops without stopping on one day this week
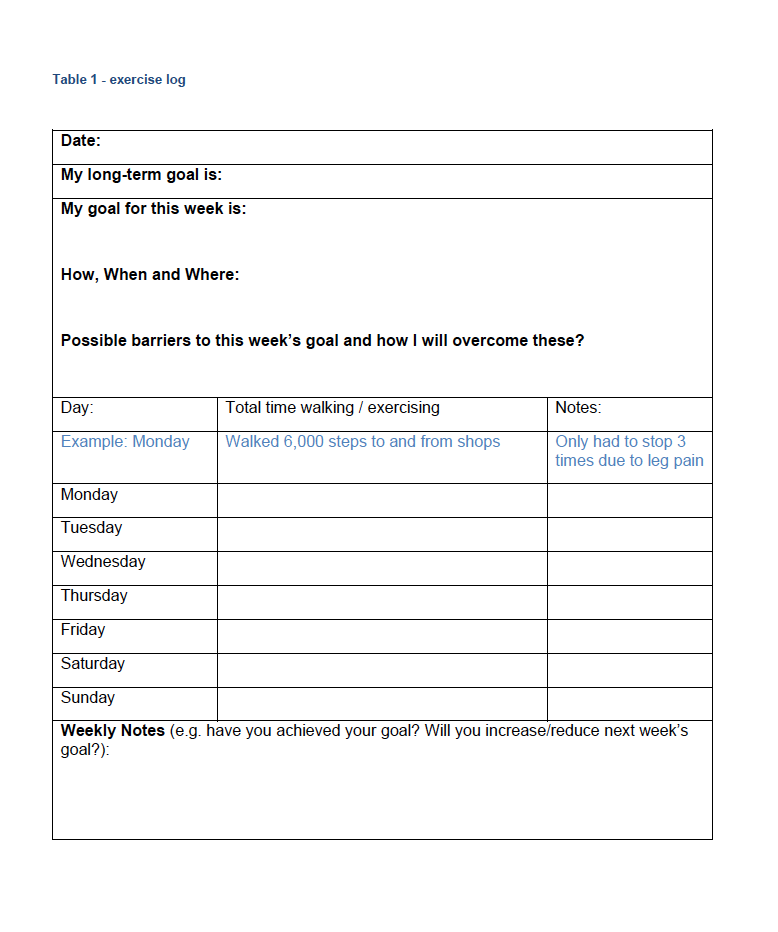
Using the table below you should set your first goal before you start this exercise programme and plan how, when and where you will achieve this. You should also consider any ‘barriers’ to completing your exercise plan and how you will overcome these.
E.g. Next week I will exercise 3 times for 30 minutes. I will do this by walking around the park on Monday and Friday afternoon and gardening at home on Wednesday morning. If the weather is bad, I will walk or garden on Tuesday afternoon instead.
Once you have achieved your goal, you should set another and create another action plan, repeating this each time a goal is met. If you find you are achieving your goals, but your leg pains are not improving then set progressively harder goals and reassess your progress after you meet them.
Monitoring progress
Setting a weekly goal and completing the table provided will help you to monitor your progress and see how much you are achieving over time.
Ways to see that you are progressing include:
-
Achieving your (progressively harder) weekly goals
-
Being able to walk further without stopping (i.e. for longer), which you can measure by taking a regular route whilst walking and reaching the next lamppost or bench before stopping.
-
Monitoring the number of steps you take using a smartphone or a pedometer or measuring how long your regular walk takes. If the number of steps you take increases or your regular walk takes less time, you have made progress.
-
You may also notice that your breathing is a little easier when exercising over time. If this is the case, you may have also improved.
Sometimes, if you need to take a little time off (because you are a little under the weather), you may notice that your progress has reduced slightly. This is normal and should not put you off exercising, you will quickly get back to where you were!
Progression
Monitoring and understanding your progress and setting goals is important, because it can motivate you to continue exercising. Also, as you notice that you have progressed, you should continue to increase your exercise efforts, to sustain or continue your improvement. This can be also be done in a number of ways:
-
Setting a more difficult weekly goal
-
On your regular walk, you might want to try to walk one lamppost or bench further before stopping.
-
If you notice that your regular walk is taking less time, you should try to increase the distance.
-
If you notice an improvement and/or can walk for 10 minutes without stopping, you should try and walk a little faster.
-
If you begin to find the same exercises a little easier (i.e. you feel less breathless), you should try to make them harder by increasing the speed or duration of these exercises.
Considerations
Although regular exercise is considered safe and adverse events are rare, it is important to understand that you are exercising unsupervised and may not have had a recent medical assessment. Therefore, by exercising according to this programme, you are doing so at your own risk. If you experience chest pain, dizziness or sickness whilst exercising, you should stop exercising immediately and seek medical advice before resuming regular exercise.
Links and resources
For more information about intermittent claudication and peripheral artery disease visit circulationfoundation.org.uk or email at: info@circulationfoundation.org.uk.
Contributors to this document:
Sean Pymer, Hull York Medical School
Saïd Ibeggazene, Sheffield Hallam University
Lindsay Bearne, Kings College London
Garry Tew, Northumbria University
Alan Hill, Patient Representative
On behalf of the UK PAD exercise professionals’ network